Is gene editing a path to the cure for HIV? Matt Chappell, who successfully underwent gene editing in order to combat human immunodeficiency virus (HIV) infection think so.
Matt Chappell who in 2014 had blood cells removed from him, disabled a gene so as to help said cells fight HIV and implanted them back into his body. Says, he is hopeful that genetic editing may well be the long-term solution to the fight against HIV and acquired immune deficiency syndrome (AIDS).
“I’ve been off medications for three and a half years,” he said. He even was able to keep the virus in check despite cancer treatments last year that taxed his immune system.
Chappell was lucky, though. Only a few of the 100 others in those experiments were able to stay off HIV drugs for a couple years; the rest still need medicines to keep HIV suppressed.
Now researchers think they can improve the treatment and are trying again to tackle HIV by doctoring DNA. New studies to test these tweaked approaches in people are getting underway.
“Gene therapy techniques have advanced greatly,” said Dr. Otto Yang of the UCLA AIDS Institute, one place working on this. “A lot of people are thinking it’s the right time to go back.”
They include Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, which is funding some of the new studies. He doesn’t think the technique will become common because millions of people do well on existing treatments. But he says it could help those who can’t easily control the virus, and should be pursued because it holds potential for a cure.
“They’re very bold, innovative techniques, mostly to try and cure people,” he said. “It’s worth trying because the science is there.”
Only one person is known to have been cured of HIV infection, a man who had a cell transplant a decade ago from a donor with natural immunity to the virus. The donor lacked a common gene that makes an entryway HIV uses to infect T cells, immune system soldiers in the blood.
The transplant gave the recipient that protection, but procedures like that are too risky and impractical for wide use. Scientists have been trying to find a way to create similar immunity by altering some of a patient’s own cells. They use a gene editing tool called zinc finger nucleases, which cut DNA at a precise spot to disable the HIV entryway gene.
The California company that makes the editing tool, Sangamo Therapeutics, sponsored the initial studies.
“It worked, the T cells were edited,” said Sangamo’s president, Dr. Sandy Macrae. But it didn’t work quite well enough: The altered T cells were outnumbered by T cells that were not altered and could still be infected.
Now, Dr. John Zaia at City of Hope, a research center in Duarte, California, is trying the approach with a twist. He’s using blood stem cells — parent cells that produce many others. Once a stem cell is altered the benefit should multiply and last longer, Zaia said.
Though the initial gene editing experiments were disappointing, there was a silver lining. Patients in those studies had a big drop in the number of cells where HIV lurked in a dormant state — the so-called reservoir of silent disease.
At Case Western Reserve University in Cleveland, Dr. Rafick-Pierre Sekaly is trying to capitalize on that drop. His study will try the same gene editing — disabling the gene that makes the HIV entryway — while keeping patients on strong antiviral medicines for at least a year before discontinuing them.
“As long as we’re not able to get rid of this reservoir, we’ll never be able to stop treatment,” he explained.
The hope is that the medicines plus the altered cells will knock down the virus and reduce the reservoir to a point where the body can control any residual disease by itself, as Chappell seems to be doing.
University of Pennsylvania scientists are trying a two-part approach: Besides knocking out the gene for the HIV entryway, they’re adding a gene to help T cells recognize and kill HIV. This second part is called CAR-T therapy, a treatment approved last year for treating cancer.
The new study’s leader, scientist James Riley, is encouraged that some patients at Penn who were in the early studies kept HIV suppressed for nearly a year without drugs.
“You’d never know they were sick” even though the virus could still be detected, Riley said. “At some point, you’re going to have confidence that it’s not going to come back.”
Chappell’s doctor, Christopher Schiessl at One Medical, a health clinic in San Francisco, hopes that’s the case for Chappell. Although he’s doing well now, Chappell is showing signs that his immune system may be weakening, Schiessl said.
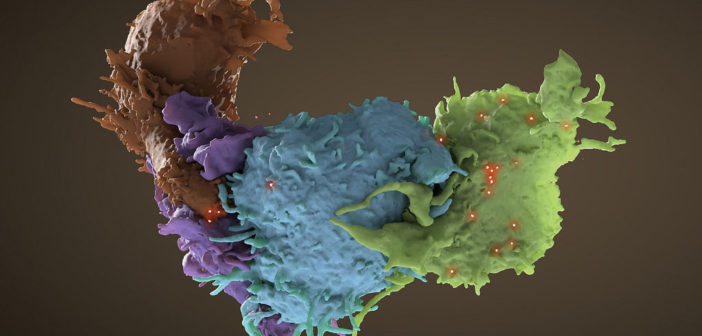
In another HIV related story, scientists at the Frederick National Laboratory for Cancer Research have discovered why some HIV patients develop AIDS faster than others. They examined the role of human leukocyte antigens, a complex of genes that varies widely from person to person and can help explain why some individuals have different immunity to infectious diseases than others.
The scientists also examined the role of two specific proteins that significantly affect the immune response to the HIV virus. The proteins — known as HLA-A and HLA-B — work together to moderate levels of HLA-E, another molecule that inhibits the activity of natural killer cells.
Those intimidatingly-named lymphocytes are critical to the body’s innate immune system, which can fight things like infection and tumors. When receptors on natural killer cells encounter and recognize high levels of HLA-E on the surface of an HIV-infected cell, the killer cell’s natural mechanism — to destroy the infected cell — is essentially turned off.
That’s a problem for patients with high levels of HLA-A and a specific variant on the HLA-B gene, which, together, lead to higher expression of HLA-E. HIV patients with those traits are less able to fight the virus because their natural killer cells are inhibited.
“You can actually measure and see that the higher HLA-A is, the higher HLA-E is,” Mary Carrington, a co-author on the paper and director of the Basic Sciences Program at the Frederick National Laboratory said. “And those patients show more rapid progression to AIDS, they have high viral loads, and they have low CD4 T-cell counts, which also help fight against infection.”
Researchers examined around 8,000 HIV-infected patients over the course of five years to help determine the role both genes play in natural killer cell inhibition. That sample included people from southern Africa, America, and Europe, who submitted genetic material for research at a time before highly effective antiviral therapy for HIV had been developed.
The high-risk genotype was found among roughly 7.8 percent of black patients and 9.6 percent of Caucasians, Carrington said. At the time when the samples were collected, none of the patients involved in the study were being treated with antiretrovirals — medication that can slow the growth of the virus and prevent it from progressing into AIDS.
With the advent of those drugs — which can prevent the growth of HIV even in high-risk patients — the role of genotype has become less important, Carrington pointed out. But even on antiretrovirals, patients aren’t cured of the virus.
“If you go off those drugs, HIV comes right back,” she said. “Even though people can live pretty normal lives while they’re on them.”